In 2019, a small group of researchers from the Peristeam Hydrotherapy Institute crowd-funded a trial study called the “Fourth Trimester Vaginal Steam Study”.
For centuries, women across the globe have used vaginal steaming to assist with postpartum recovery. This practice is experiencing a resurgence in popularity in the US but obstetricians and gynecologists remain largely unfamiliar with the practice and are unequipped to provide informed advice to their patients on its safety and efficacy. For this reason, clinical studies on vaginal steaming are in high demand.
The following study was designed to provide a foundational exploration of the impact of vaginal steaming on postpartum recovery.
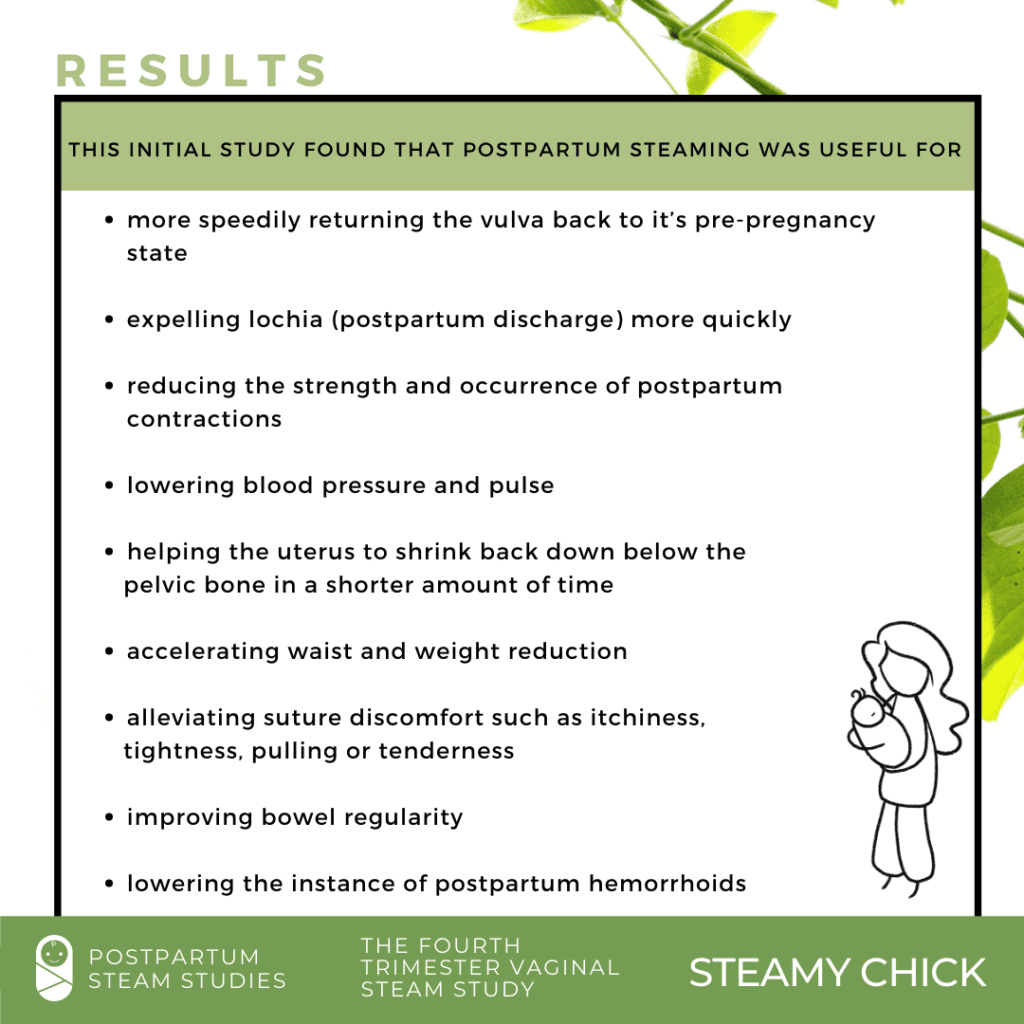
This initial study found that postpartum steaming was useful for more speedily returning the vulva back to it’s pre-pregnancy state; expelling lochia (postpartum discharge) more quickly; reducing the strength and occurrence of postpartum contractions; lowering blood pressure and pulse; helping the uterus to shrink back down below the pelvic bone in a shorter amount of time; accelerating waist and weight reduction; alleviating suture discomfort such as itchiness, tightness, pulling or tenderness; improving bowel regularity; and lowering the instance of postpartum hemorrhoids.